Cubans adopt solar energy as blackouts and fuel shortages deepen crisis
Cubans are increasingly turning to solar power to keep businesses operating and basic household appliances running during prolonged electricity cuts, ...
The United States has long been at the forefront of medical advancements, yet its healthcare system remains one of the most expensive and least accessible among developed nations
In 2023, healthcare spending reached $4.9 trillion, making up 17.6% of the country’s GDP.
Despite this investment, millions of Americans continue to face challenges in affordability and access, sparking a long-running debate: Is healthcare a public necessity, or an economic industry driven by profit?
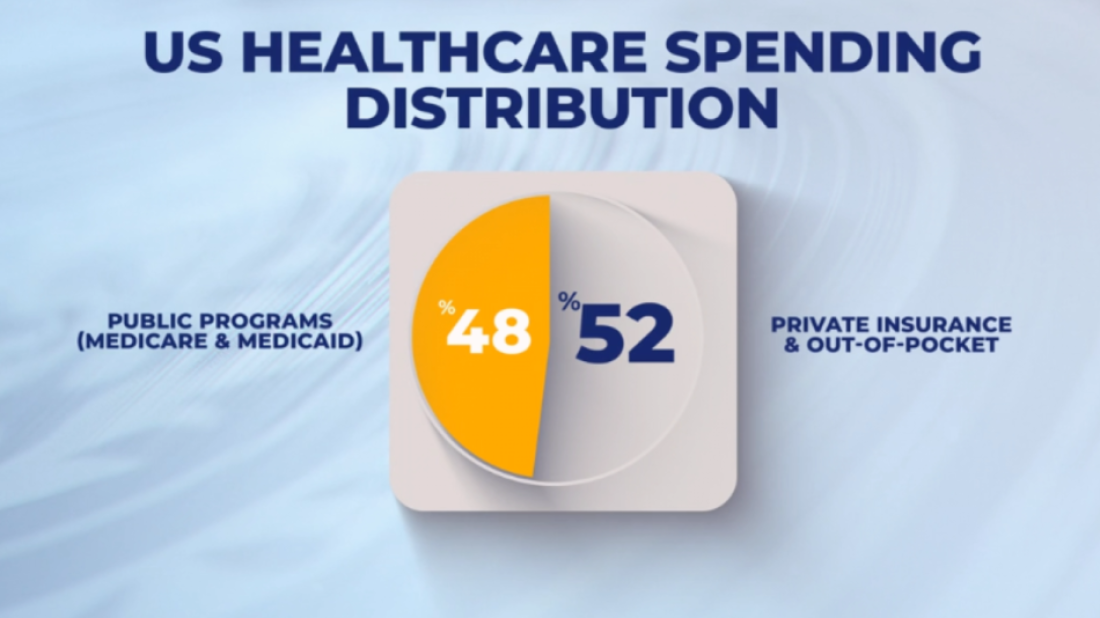
Unlike many nations that operate under universal healthcare systems, the U.S. relies on a hybrid model, where public programs like Medicare and Medicaid cover 48% of spending, while private insurance and out-of-pocket costs make up the rest. While this structure provides flexibility, it has also led to rising costs, disparities in care, and financial strain on individuals.
With every presidential election, healthcare reform takes center stage. Policies have been introduced, debated, and adjusted—but has the system truly changed?
The Influence of Insurance Companies
At the heart of the U.S. healthcare system lies the private insurance industry, which plays a defining role in coverage, pricing, and accessibility.
Major companies such as UnitedHealth Group, CVS Health, and Anthem generate hundreds of billions in annual revenue, shaping the system through pricing structures and lobbying efforts.
UnitedHealth Group alone has spent over $30 million in lobbying during recent election cycles, influencing policy decisions. Critics argue that this level of corporate involvement blurs the line between healthcare as a service and healthcare as a business, often making affordability a secondary concern.
When Healthcare Becomes an Industry
Once driven by nonprofit institutions, the U.S. healthcare system has evolved into a multi-billion-dollar industry, where treatment costs can fluctuate dramatically based on location, hospital policies, and corporate pricing strategies.
Consider Jeffrey Kivi, a high school teacher who relied on Remicade infusions to treat an autoimmune condition. Initially, his treatment cost $19,000 per month, but after his doctor switched hospitals, the price surged to $132,000 per month—a reflection of hospital fees, patents, and market dynamics.
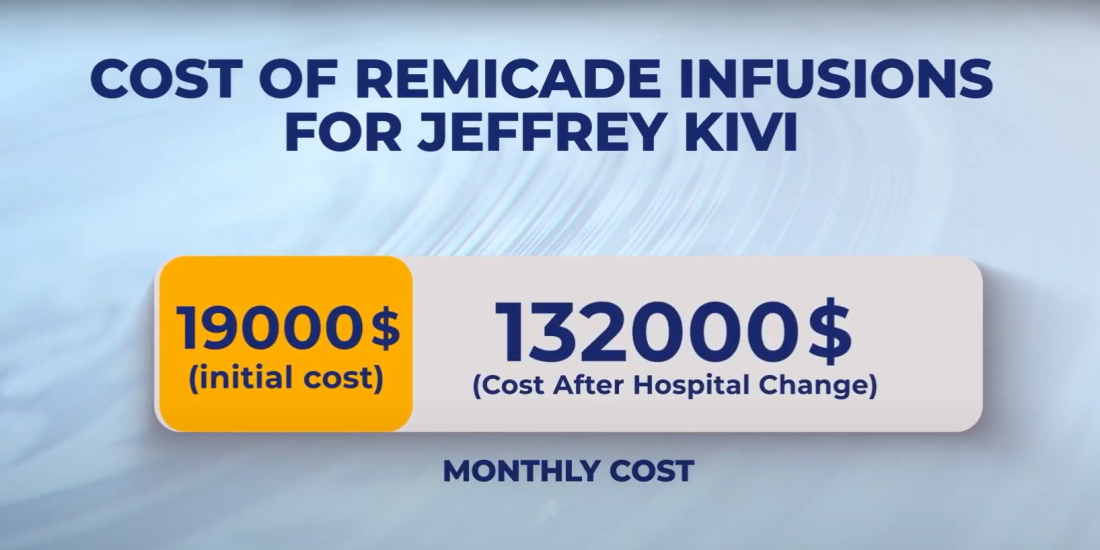
His case, detailed in Elisabeth Rosenthal’s book An American Sickness, is not an isolated one. Similar cost-cutting measures have been introduced by insurance companies, sometimes sparking backlash. Anthem Blue Cross once proposed limiting anesthesia coverage based on surgery duration, a policy that raised concerns about patient safety before it was eventually withdrawn.
While the healthcare sector generates significant revenue, the question remains: Are resources being allocated in ways that genuinely improve patient care?

The Global Perspective: Spending vs. Outcomes
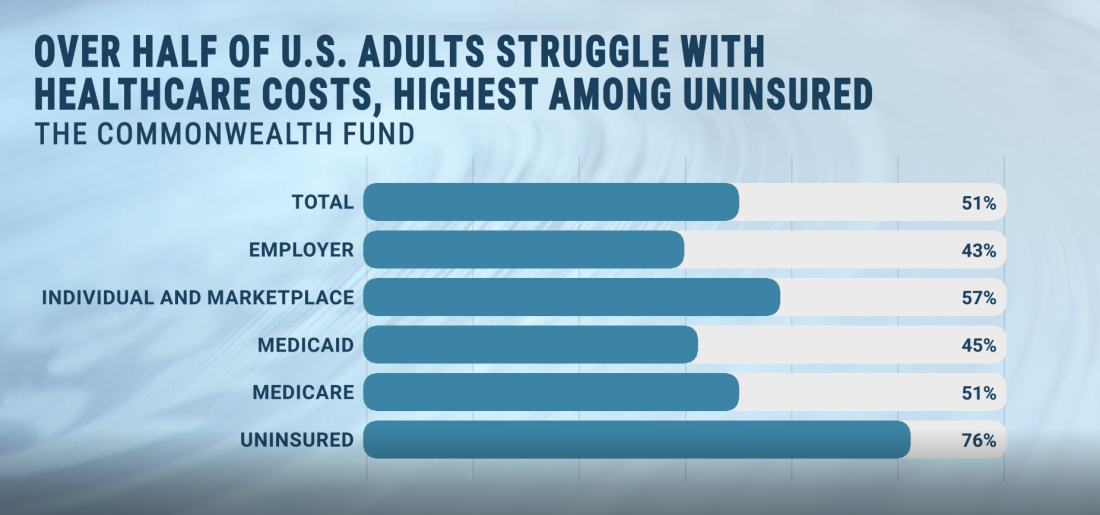
A recent study by The Commonwealth Fund, Mirror, Mirror 2024, ranks the U.S. lower than many developed nations in key healthcare indicators:
Life expectancy in the U.S. remains below the average of peer countries.
Preventable deaths occur at higher rates than in comparable nations.
Healthcare costs continue to far exceed those of countries with universal coverage.
Meanwhile, countries like the Netherlands, Australia, and the U.K. achieve better health outcomes at lower costs, prompting ongoing discussions about whether the U.S. should rethink its approach.
At the same time, U.S. health insurance companies contribute over $100 billion in corporate taxes annually, leading to debates on whether such revenues should be redirected toward affordability and accessibility efforts.
Critics also point to broader budget priorities, as the U.S. allocates over $800 billion annually to its military. This has fueled discussions on whether a rebalancing of national spending could better support domestic healthcare initiatives.
The Future of Healthcare: Reform or Status Quo?
The structure of U.S. healthcare continues to evolve, yet the fundamental issues of cost and accessibility remain unresolved.
Newly elected President Donald Trump has introduced proposals focused on reducing drug prices and increasing transparency, though their long-term impact remains to be seen.
As policymakers debate cost controls, corporate influence, and national spending priorities, the central question persists: Health or wealth?
The balance between economic interests and patient care will define the future of healthcare in America.
The drumbeats have finally faded at the Marquês de Sapucaí, bringing the competitive phase of the Rio Carnival 2026 to a dazzling close. Over two marathon nights of spectacle, the twelve elite schools of the "Special Group" transformed the Sambadrome into a riot of colour.
Israel is preparing for the possibility of receiving a green light from the United States to launch strikes against Iran’s ballistic missile system, according to Israel’s public broadcaster KAN.
Aghdam’s Qarabag FK experienced a 6–1 defeat to England’s Newcastle United in the first leg of their UEFA Champions League play-off tie in Azerbaijan's capital Baku Wednesday evening (18 February).
Qarabağ FK are facing Newcastle United in the UEFA Champions League play-off round on Wednesday evening in Baku, in what will be the first UEFA competition meeting between the two clubs.
Start your day informed with AnewZ Morning Brief: here are the top news stories for the 18th of February, covering the latest developments you need to know.
Cubans are increasingly turning to solar power to keep businesses operating and basic household appliances running during prolonged electricity cuts, as fuel shortages make diesel generators and other temporary solutions more difficult and costly to maintain.
Mexican authorities have uncovered a 22-metre tunnel used to siphon fuel from a state-owned pipeline, shedding light on the country’s long-running battle against a lucrative black-market trade often controlled by organised crime.
At least four people have died and 17 others were injured after a liquid gas truck overturned and exploded in Santiago, Chile’s capital, authorities confirmed on Thursday. Police said the driver was among those killed.
Day 13 of the Milano Cortina 2026 Winter Olympics featured decisive finals, thrilling performances and packed arenas across Milan, Livigno, and Cortina d’Ampezzo. The Games combined precision, speed, and drama, marking another memorable day in the Winter Olympics.
Gianni Infantino, president of the Fédération Internationale de Football Association (FIFA), announced a new partnership with the Board of Peace on Thursday (19 February), committing to build football pitches and arenas in Gaza as part of broader efforts to rebuild the region.
You can download the AnewZ application from Play Store and the App Store.

What is your opinion on this topic?
Leave the first comment